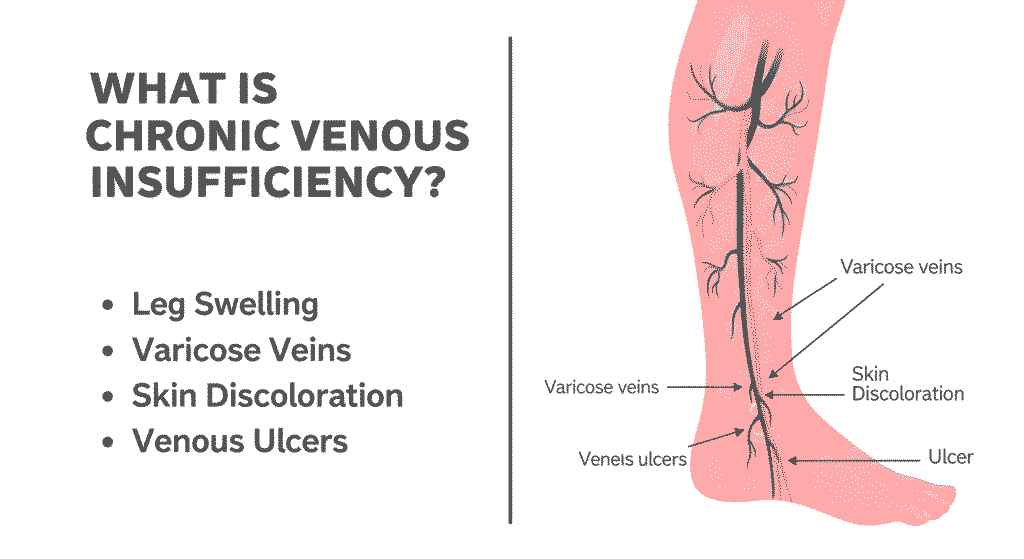
Chronic venous insufficiency (CVI) affects millions of Americans, causing discomfort and, if untreated, serious complications. It occurs when leg veins fail to efficiently return blood to the heart, leading to symptoms like swelling, varicose veins, and even skin ulcers. Often mistaken for a cosmetic issue, CVI is a medical condition requiring proper diagnosis and management. This guide explores its causes, symptoms, treatments, and recent developments to help you understand and address this condition.
How It Happens: The Science Behind Chronic Venous Insufficiency
Veins rely on one-way valves to direct blood toward the heart. In CVI, these valves weaken or become damaged, allowing blood to flow backward (venous reflux) and pool in the lower legs. This increases venous pressure, leading to swelling, pain, and skin changes. Over time, untreated CVI can impair circulation, affecting vein health and quality of life. Understanding this process is key to recognizing the need for early intervention.
Causes and Risk Factors of Chronic Venous Insufficiency
Several factors contribute to CVI development:
- Age: Risk rises after age 50 due to natural vein wear.
- Gender: Women face higher risk from hormonal changes, pregnancy, or birth control.
- Obesity: Excess weight strains leg veins.
- Prolonged sitting or standing: Jobs requiring long immobility periods worsen vein function.
- Genetics: A family history of vein disorders increases susceptibility.
- Deep vein thrombosis (DVT): Past blood clots can damage vein valves.
- Pregnancy: Higher blood volume and vein pressure elevate risk.
Lifestyle and medical history play significant roles in CVI onset.
Symptoms of Chronic Venous Insufficiency
CVI symptoms often start subtly but worsen without treatment. Common signs include:
- Swelling in legs or ankles, especially after standing
- Aching, heavy, or cramping legs
- Visible varicose veins (bulging, twisted veins)
- Itchy or leathery skin
- Skin discoloration, often brownish around ankles
- Venous ulcers (slow-healing sores)
These symptoms can disrupt daily life, particularly in advanced stages, making early recognition critical.

Diagnosis: How Chronic Venous Insufficiency is Identified
Diagnosing CVI begins with a physical exam and medical history review. The primary diagnostic tool is duplex ultrasound, a non-invasive test that visualizes blood flow and vein structure. In complex cases, doctors may use venography to assess deeper veins. Accurate diagnosis ensures tailored treatment, preventing progression. Consult a vascular specialist for thorough evaluation.
Treatment Options for Chronic Venous Insufficiency
CVI is manageable with a range of treatments aimed at improving circulation and relieving symptoms:
- Compression stockings: Elastic socks apply pressure to enhance blood flow, reducing swelling.
- Lifestyle changes: Weight loss, regular exercise (e.g., walking), and leg elevation help symptoms.
- Medications: Diuretics reduce swelling; some drugs improve vein tone.
- Minimally invasive procedures:
- Sclerotherapy: Injects a solution to close small veins.
- Endovenous laser therapy (EVLT): Uses laser to seal larger veins.
- Radiofrequency ablation (RFA): Applies heat to close affected veins.
- Surgical options: Vein stripping or bypass for severe cases.
Per the American Vein & Lymphatic Society, minimally invasive treatments boast a 90%+ success rate when performed by specialists.
Prevention Tips: How to Lower Your Risk of CVI
While not fully preventable, these habits reduce CVI risk:
- Avoid prolonged sitting or standing; take breaks to move.
- Exercise regularly to boost leg circulation.
- Maintain a healthy weight to reduce vein pressure.
- Elevate legs above heart level for 15–30 minutes daily.
- Avoid tight clothing around the waist or legs.
- Wear compression stockings if at risk (e.g., during pregnancy or long flights).
Proactive steps can significantly protect vein health.
Real-World Relevance: President Trump Diagnosed with CVI
In July 2025, former President Donald Trump was diagnosed with CVI after experiencing leg swelling and bruising, as reported by Reuters and AP News. Duplex ultrasound confirmed the diagnosis, ruling out blood clots or arterial issues. His case, managed with compression therapy and lifestyle adjustments, has spotlighted CVI, raising awareness about its prevalence among older adults. Experts note Trump’s stable health underscores CVI’s manageability with proper care. Learn more about vascular health in public figures.
When to See a Doctor
Seek medical advice if you experience:
- Persistent leg swelling or pain
- Skin discoloration or texture changes
- Varicose veins
- Slow-healing leg sores
Early intervention prevents complications like ulcers or infections. Contact a vascular specialist for evaluation.
FAQs About Chronic Venous Insufficiency
Q1: Is chronic venous insufficiency dangerous?
Untreated CVI can lead to painful ulcers, infections, or reduced mobility but is rarely life-threatening.
Q2: Can chronic venous insufficiency go away on its own?
No, CVI typically progresses without treatment. Early management is essential.
Q3: Who is most at risk for CVI?
Older adults, women, those with family history, or sedentary lifestyles face higher risk.
Q4: What is the difference between CVI and varicose veins?
Varicose veins are a symptom of CVI; not all cases indicate CVI, but they can signal early vein issues.
Q5: Can men get chronic venous insufficiency?
Yes, men are affected, particularly with age or risk factors like obesity or DVT.
Conclusion
Chronic venous insufficiency impacts nearly 40% of Americans over 50, per Cleveland Clinic, but is highly treatable with timely care. From compression therapy to minimally invasive procedures, effective options exist to manage symptoms and prevent complications. High-profile cases, like former President Trump’s 2025 diagnosis, have boosted awareness, encouraging more Americans to prioritize vein health. If you suspect CVI, consult a doctor to explore treatment and take control of your vascular wellness.
For more news and update stay tuned with usamainland.com